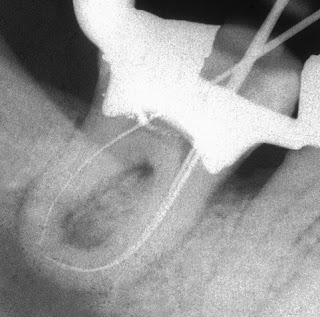
 How many people would like to finish the above case in one visit?
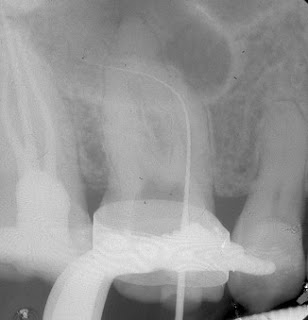
How many people would like to finish the above case in one visit?Or the case below, for that matter.
 I think the first point of consideration is not how many visit endo should be finished in?
I think the first point of consideration is not how many visit endo should be finished in?Technical quality of endo treatment is of paramount importance. First consideration is, therefore, whether you can achieve adequate technical quality of endo treatment?
By adequate technical quality I mean;
Diagnosis and treatment plan properly formulated? Rubber dam used and properly applied? All root canal located? Working length correctly determined? Antibacterial irrigant used? MAF large enough? Radiographically, your root filling appears in appropriate length, density and taper? and so on…
If you could achieve all those, but it needs more than one visit to achieve it, then why on earth would you want to finish endo in one visit and, of course, with technical inadequacy.
Now, assume that adequate technical quality can be achieved in one visit. Is there any reason why the treatment shouldn’t be completed?
If you wanted to kill bacteria with calcium hydroxide dressing, it would take at least a week for calcium hydroxide to work effectively (Sjogren et al. 1991). That means you can’t complete the case in one visit.
Is calcium hydroxide dressing necessary?
To answer this question, one more issue needs to be clarified.
There are two separate entities in endodontics. A tooth WITH and WITHOUT apical periodontitis (apical radiolucency).
To make it short, I need to simplify it a bit. A tooth without apical periodontitis (normal vital tooth (elective endo) or irreversible pulpitis) is considered not infected. Or infection hasn’t been established, at least, at the apical part of the canal in case of irreversible pulpitis. There’s no bacteria in the canal at the first place, therefore, endo tx shouldn’t be aiming to reduce a number of bacteria. Make sense? So calcium hydroxide dressing is not necessary in these cases and, as a result, one visit endo could be done, provided that adequate technical quality could be achieved.
A tooth with apical periodontitis is infected (Sundqvist 1976). Apical periodontitis is caused by bacteria (Kakehashi et al. 1965; Moller et al. 1981), so endo tx in this case should be aiming to reduce as much a number of bacteria as possible.
The higher the number of canals that can be rendered bacterial negative, the higher the chance of healing (Sjogren et al. 1997).
Mechanical instrumentation + NaOCl irrigant = 40-60% of the treated teeth bacteria-negative (Bystrom et al. 1983; Shuping et al. 2000).
Mechanical instrumentation + NaOCl irrigant + calcium hydroxide dressing for at least a week = roughly around 70% (weighted average of the following five studies) of the treated teeth bacteria-negative (Orstavik et al. 1991; Peters et al. 2002a; Shuping et al. 2000; Sjogren et al. 1991; Yared et al. 1994)
By extrapolation, including calcium hydroxide dressing between appointments should provide a higher healing rate, because bacteria are further reduced.
In conclusion, one visit can be done in a tooth without apical periodontitis (there’s no controversy about it). Calcium hydroxide dressing should be included in the treatment of a tooth with apical periodontitis (or a tooth with established infection), so one visit endo is biologically and logically not possible (there’re some controversies surrounding this case, though).
Controversial issue:
Even though, it does make biological sense to include calcium hydroxide to the treatment of teeth with apical periodontitis as I outlined the logical step above. Randomized controlled clinical trials (the best design of clinical study to test treatment effectiveness) have failed to show the clinical benefits of calcium hydroxide dressing in terms of healing rate (Peters et al. 2002b; Trope et al. 1999; Weiger et al. 2000).
Why have benefits of calcium hydroxide not been shown in these studies?
Endodontic treatment is skill-dependent procedure (as with any surgical procedures). Operator skill and/or settings could affect treatment outcome (healing rate) to some extent. It has been conjectured that these researchers (Peters, Trope, and Weiger) are experienced endodontists, their treatment technical qualities must be high.
Therefore, the additional benefits of calcium hydroxide are small in comparison to the rest of the treatment and could not be easily shown statistically. On the other hand cleaning, shaping, and obturation by novice operators (low skill level expected) could well be benefited from calcium hydroxide medication as another layer of antibacterial process. In this scenario multiple-visit endodontics with inter appointment calcium hydroxide medication might significanly show better results than single-visit endodontics.
Reference:
Bystrom A, Sundqvist G (1983) Bacteriologic evaluation of the effect of 0.5 percent sodium hypochlorite in endodontic therapy Oral Surgery, Oral Medicine, Oral Pathology 55, 307-12.
Kakehashi S, Stanley H, Fitzgerald R (1965) The effect of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surgery Oral Medicine Oral Pathology Oral Radiology & Endodontics 20, 340-9.
Moller AJ, Fabricius L, Dahlen G, Ohman AE, Heyden G (1981) Influence on periapical tissues of indigenous oral bacteria and necrotic pulp tissue in monkeys Scandinavian Journal of Dental Research 89, 475-84.
Orstavik D, Kerekes K, Molven O (1991) Effects of extensive apical reaming and calcium hydroxide dressing on bacterial infection during treatment of apical periodontitis: a pilot study International Endodontic Journal 24, 1-7.
Peters LB, van Winkelhoff AJ, Buijs JF, Wesselink PR (2002a) Effects of instrumentation, irrigation and dressing with calcium hydroxide on infection in pulpless teeth with periapical bone lesions International Endodontic Journal 35, 13-21.
Peters LB, Wesselink PR (2002b) Periapical healing of endodontically treated teeth in one and two visits obturated in the presence or absence of detectable microorganisms International Endodontic Journal 35, 660-7.
Shuping GB, Orstavik D, Sigurdsson A, Trope M (2000) Reduction of intracanal bacteria using nickel-titanium rotary instrumentation and various medications. Journal of Endodontics 26, 751-5.
Sjogren U, Figdor D, Persson S, Sundqvist G (1997) Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis International Endodontic Journal 30, 297-306.
Sjogren U, Figdor D, Spๅngberg L, Sundqvist G (1991) The antimicrobial effect of calcium hydroxide as a short-term intracanal dressing International Endodontic Journal 24, 119-25.
Sundqvist G (1976) Bacteriological Studies of Necrotic Dental Pulps. Umea Sweden: Umea University Odontological Dissertations no. 7.
Trope M, Delano EO, Orstavik D (1999) Endodontic treatment of teeth with apical periodontitis: single vs. multivisit treatment. Journal of Endodontics 25, 345-50.
Weiger R, Rosendahl R, Lost C (2000) Influence of calcium hydroxide intracanal dressings on the prognosis of teeth with endodontically induced periapical lesions. International Endodontic Journal 33, 219-26.
Yared GM, Dagher FE (1994) Influence of apical enlargement on bacterial infection during treatment of apical periodontitis Journal of Endodontics 20, 535-7.
